This post first appeared on , in September 2016.
TL;DR
About a year ago, I was diagnosed with testicular cancer. About a week ago, my CT scans still showed no signs of metastasis. That’s great, and my general experience up to now was as pleasant as possible. This post is to provide other graduate students with the inside experience of being diagnosed with cancer during your PhD, and to highlight some of the issues I’ve noticed along the way. Most importantly, students with serious illnesses generally aren’t supported very well by their grant, cancer has some unexpected mental side-effects, and people should stop referring to it as a ‘fight’.
Disclaimer: This is my story; your experience may differ.
Diagnosis
To put it bluntly, I woke up with a nasty ache in my nuts one day. It didn’t subside during the day (cycling to work didn’t help!), so I scheduled an appointment with my GP. The next day, the pain got worse, and I phoned the doctor’s office to ask whether I could come in directly. At this point, my testicle was about the size of a chicken egg, and I was genuinely concerned.
The first time someone other than a romantic partner asks you to pull down your trousers is a bit weird. Even more so in this case, as a medical student was present: This guy was of my age and went to my university, and was now examining my testicles. What’s interesting, though, is how quick the initial weirdness fades. Medical professionals see these things all the time, and your junk isn’t going to be very different from somebody else’s. No big deal. At this point, the number of people who have touched my genitals for medical reasons is greater than the number of people that have touched them for recreational purposes. I realise that the idea of a stranger seeing and examining your crown jewels can put men off seeing their doctor, but seriously, take it from an experienced patient: Go see your GP if you think something is amiss.
In my case, the doctor pointed out to me and his student, that my giant ball was likely caused by an infection-related build-up of fluids. He prescribed some antibiotics, and asked me to come back in two weeks. The course of antibiotics removed the pain, but didn’t decrease the swelling. So after re-examining my chicken egg, the GP referred me to a urologist. You should know that testicular cancer is really incredibly rare: the incidence in Western countries is only between 1 and 8 people in 100 000 [1], although it does seem to be on the rise [2]. So it’s completely reasonable that my GP initially thought of something else.
After seeing an ultrasound scan of my scrotum, the urologists first words were “Well, there’s no easy way of saying this: You have cancer.” I appreciated his frankness, but was too flabbergasted to fully appreciate the gravity of what he had said. Of course, I had spent some time Googling the potential causes of suddenly increased trouser-bulges. My conclusion had been that cancer would be very unlikely, and I even felt comfortable enough to joke about it. The urologist explained the biology behind testicular cancer, and briefly went over what the next few weeks would bring. My only real concern was with the survival rate, and I vaguely recall asking about it several times. Pro-tip: Bring a notebook to every doctor’s appointment, because retaining information is incredibly challenging in these situations.
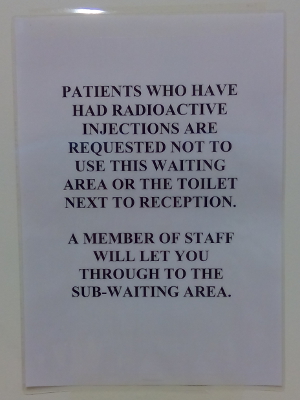
The urologist left me with a wonderful specialist uro-oncology nurse, who explained to me that there would be blood tests, an operation, more blood tests and a CT scan, and that we would only really know how serious the cancer was after the results of those tests were in. This is where the first mental challenge starts: You’ve just been told you have cancer, but you won’t know whether it has spread throughout your body until several weeks from now. The suspense is terrible.
Finding your way through cancer
The treatment of testicular cancer is very stereotyped: An operation is performed to remove the affected testicle, a biopsy is performed on the removed tumour to establish what type of cancer you have, and a CT scan of your abdomen and chest should show how far the cancer has spread. If the cancer has spread, you receive several courses of chemotherapy. How many courses and what type of chemo depends on the type of tumour. In general, the survival rates are high. Testicular cancer is the lighting example in oncology, because platinum-based chemotherapy has greatly increased the likelihood of surviving, and curing patients is now actually a realistic possibility. That’s your tax and charity money at work!
As a newly-diagnosed patient, you read about this information on all sorts of leaflets and websites, but all you think is “OH MY GOD, I’M SURE I HAVE THE WORST CANCER EVER, AND I’M GOING TO DIE!“. At least, that’s what I thought, and I’ve since learned that this is a very common response. If you’re reading this because you’re in a similar situation, I would strongly recommend joining MacMillan’s Online Community, where patients and other affected people (friends/family) can exchange experiences and information. There are communities for almost every type of cancer, and they are a great place to ask all your questions, and to talk about your fears and anxieties about what’s to come. If you Google stuff, you will browse through websites until you find one that tells you that you are likely to die. If you ask about the same thing on the support forum, you usually receive more up-to-date and realistic information.
Although you initially greatly over-estimate the chance that your disease will kill you, there is no denying that it is a possibility. Especially when you’re young, that’s not a pleasant realisation. Coping with your mortality is a very personal experience, and I don’t think there is a perfect way of doing it. For me, complete and utter nihilism actually really helped. Imagine the universe a billion years from now. You’re not in it, your loved ones aren’t in it, and even your planet isn’t in it. Heck, at some point, not even warmth will be in the universe anymore. The inevitability of this outcome makes whatever you do completely futile. On a smaller scale, you will cease to exist when your brain dies. That means you won’t be able to think about anything anymore, nor relive any memory. Once you’re dead, that’s it for you. So it doesn’t matter how and how long you’ve lived; at the end of it, it will be reduced to nothing anyway. To me, that’s not depressing, it’s liberating. I don’t have to create a legacy (there won’t be any left at some point), and I don’t have to be too concerned with the future (it’ll end anyway), so I can spend my days doing whatever.
Before anything was done to me, I was advised to store some sperm. Cutting out one of your testicles doesn’t necessarily render you infertile, but chemotherapy will. Usually, your fertility will recover, but there is a chance it will be gone forever. Storing sperm is a surreal experience. You’re asked about what you’d like to happen to your deposit in the event of your death. Are you comfortable enough for your partner to use it if you die? And what is your long-term plan, in the event you live long enough to produce offspring? Will it be possible to transport the stored sperm to a different facility, even when that is in a different country? (Yes!) And how much does it cost? (Around 200-300 pounds a year.) After having that conversation, you’re led into a room that is somehow exactly like you expect it to be. Leather couch with metal accents, dirty magazines in a corner, tissues everywhere. The following pictures tell the whole story, really. Walking into this room was the first time I laughed since the diagnosis three days earlier.
The actual operation, an orchiectomy, isn’t too bad. An incision is made in the groin (much like with a hernia), the blood and lymph vessels in spermatic cord are clamped (to prevent bits of the tumour from spreading during surgery), and I imagine the testicle is pulled and pushed out. Urologists have to do a certain number of these procedures per year to be allowed to do them, so they will be competent. The whole things takes less than an hour, and you are usually allowed to go home on the same day. Unfortunately, I wasn’t, because my operation happened in the early evening (late schedule, running even later). The upside of this was that hospital food tasted great after not eating for a day!
Staying on a ward is weird, though. All other patients were worse off than me, and made noises of agony. There was also a demented patient down the hall, who was probably scared and disoriented. He screamed throughout the night, and fought the nurses. Even after being there for just one night, I’ve gained a lot of respect for them. They do an amazing job in very difficult circumstances.
Some random advice for fellow patients: You will spend a lot of time waiting around. Bring a book, but be careful about which one. I read On the Move, Oliver Sacks’ autobiography, and that was a mistake. Don’t get me wrong, the book is great. But a few pages in, Sacks describes that when he was a pre-med student, a fellow Oxford student (like myself) came to him with a medical issue. His testicle had swollen to the size of an egg (like mine). Sacks told the guy that he might have testicular cancer (again, like me!), and that he should visit a doctor. Turns out he did have cancer, and died soon after (F*CK, THAT COULD BE ME!). It doesn’t end there, as a lot more people die of cancer in that book. Not very uplifting to read, if you’re still unsure about your own faith.
I was lucky: There were no signs of metastasis in my biopsy or my post-op CT scan. My blood levels also returned to normal. That does not mean it’s all hunky-dory; it could be the cancer has spread, but that it’s not detectable on scans or in the blood yet. That’s a terrifying thought, and I’ll return to that later. For now, the oncologists advised me to go on a surveillance trajectory. When the cancer does show up, they can always start chemo. If it doesn’t, then there’s no need for future treatment. Chemotherapy has many nasty side-effects, including death by infection during the treatment, and also an elevation of your chances of getting more cancers. Avoiding it when it’s not necessary is best.
As a final note on the treatment, I would like to add that the ‘fighting’ metaphor for dealing with cancer is awful. I get that it’s appealing, as it can make you feel as though you (or your loved one) has some control. But, unfortunately, it doesn’t work like that. You don’t ‘fight’ cancer. You suffer from a stochastic and massively complex process, and whether you make it through isn’t up to you. It is in some way, as you choose to adhere to your treatment regime or not, but you won’t overturn your cancer by wanting it real bad. Keeping your chin up and being positive is great, and has been shown to be relate to how you will feel throughout and after your illness [3]. But the downside of the fighting metaphor, is that it inherently suggests that you can ‘lose’ if you didn’t fight enough. That’s simply not true: Very strong people die of cancer, and none of them by fighting too little. As an alternative, I love how Maggie’s Centres phrase it on their information posters: “Finding your way through cancer“. This is much truer to what the actual process is like, whether it ends in death or not.
In remission?
So, you’ve had an operation, probably chemotherapy, and your test results come back negative. Are you out of the woods now? People ask this regularly, and the answer is more complex than you might think. In fact, you just don’t know. Before the operation, some cancerous cells might have spread to other parts of your body. These cells can start to form secondary tumours where they land. Initially, these tumours will not be large enough to show up on CT scans, and they won’t produce enough tumour markers for blood tests to pick up. How quickly these secondary tumours grow depends on what their surroundings are like. If they don’t have a good food supply, it can take years for them to slowly grow large enough to show up. So most patients in remission could have a little tumour growing in them, just waiting to rear it’s ugly head.
Randall Munroe catches this feeling really well in his xkcd comic ‘Lanes’ (also included below). Knowing that something might still be growing inside of you can be rather disturbing, as this video clearly illustrates. This is another major mental challenge, as it can make you incredibly sensitive to potential symptoms. Abdominal pain? It’s probably spread to your lymphs there. A cough? Yep, it’s in your lungs now. Swollen lymph nodes in your neck? Oh, no, it’s in your neck; so it’s probably also in your brain now.
I was never a hypochondriac. In fact, before my testicular issues, I had only been to the GP twice in my adult life. Since being diagnosed with cancer, I involuntarily pay more attention to my body. If something feels amiss, I immediately think “Oh, no, it has spread”, often before I’m even fully aware of the actual issue. It takes a conscious effort to suppress this kind of thinking. In addition, I’ve learned that knowing about psychosomatic processes does not make you immune to them. When I worry about abdominal or neck lymphs, I’ll have abdominal or neck pains soon after. I know that I’m imagining things, but that doesn’t stop it from happening. The mind is a powerful thing, and it’s fascinating to witness these processes from a patient perspective.
Academic consequences
As a PhD student, I have three years to finish my thesis. In order to do this, I need to do research: conduct experiments, analyse my data, write up my results; rinse and repeat. Three years is a short time to produce a lot of good work, especially since a large part of every PhD is learning all sorts of new techniques (handling specific equipment, analysing data with certain methods, programming, and so on). PhD students are part of a university department, and they are supervised by a senior academic. The experience is very similar to being a junior employee in any other job. Despite working full-time (and often more) and doing a lot of work for the department, PhD students are not normally considered to be an employee. Instead, they are students who receive a stipend instead of a salary.
Having a student status does not only mean you earn less money than your working peers do, it also means you have less rights. If everything goes along smoothly, that is no issue: It’s good fun to be expected to act as a student a bit longer, and you can do good work even without having a decent employment contract. However, when a graduate student is faced by a serious illness, things start to break down. This is painfully apparent in the Grant Terms and Conditions from Research Councils UK [4]. Clause 58 reads “The Research Organisation must make suitable arrangements for coping with absences of students for illness, maternity leave, Ordinary Paternity Leave, shared parental Leave, adoption leave, extended jury service and holidays“. This points to the university to make arrangements for ill students. However, these illnesses are only expected to be 13 weeks or less. Clause 60: “Payment of a studentship can continue for absences covered by a medical certificate for up to thirteen weeks within any 12-month period. If the illness lasts, or is expected to last, for more than thirteen weeks, the Research Organisation should make arrangements to suspend the studentship“.
So if you have cancer and require surgery and chemotherapy, your stipend is likely to be suspended. The same regulations also discourage other employment: clause 38 forbids full-time employment, and points out that part-time employed students are only eligible for part-time awards. This means that their stipend is most likely a PhD student’s only livelihood. Having that suspended because you’re seriously ill, means that you need serious financial reserves, or face being homeless and hungry.
To put this in perspective: PhD students are typically in their mid-twenties or early thirties, and academic peers with a staff contract are allowed up to 6 months of paid sick leave. I was one of those lucky bastards, as my grant comes from the European Commission’s Marie Sklodowska-Curie programme. This requires the university to sign PhD students onto a staff contract. Thanks, EU!
I don’t have to point out that suspending PhD students’ livelihood when they get cancer or any other serious illness is not OK. Research Councils in the UK, and equivalent funding sources elsewhere, should revise their rules.
Acknowledgement
I thought about acknowledging all the wonderful people who have helped and supported me during the past year, but I decided against it. Not because I’m ungrateful, but because I can’t fit the names of all those people that I’m grateful to on here. You’re all the best.
There is one person I would like to mention by name, and that is Rabea Nourbakhsh. She is the mother of a friend and colleague of mine, and she was diagnosed with brain cancer a little over a year ago. Although I never met her, I felt connected through our diseases, through her daughter, who was an amazing support to her and to me. (Your green drinks tasted so awful, they must have been super healthy!) Sadly, Rabea suffered from a very aggressive brain tumour, and she passed away recently. The reason I mention her by name here, is that her amazing family are honouring her last plans to raise money for the medical aid of refugees in the Middle East. Her website is in-her-memory.com, if you’d like to know more.
References
- Adami et al. (1994). Testicular cancer in nine northern european countries. International Journal of Cancer, 59(1), p. 33-38. doi: 10.1002/ijc.2910590108
- Huyghe et al. (2003). Increasing Incidence of Testicular Cancer Worldwide: A Review. Journal of Urology, 170(1), p. 5-11. doi: 10.1097/01.ju.0000053866.68623.da
- Spiegel, D. (1997). Psychosocial aspects of breast cancer treatment. In Seminars in Oncology-Supplements (Vol. 24, No. 1, pp. 36-47). New York, USA: Grune & Stratton.
- Research Councils UK (2014). Conditions of Research Council Training Grounds. Retrieved from: www.rcuk.ac.uk/funding/grantstcs. Click here for a PDF version.
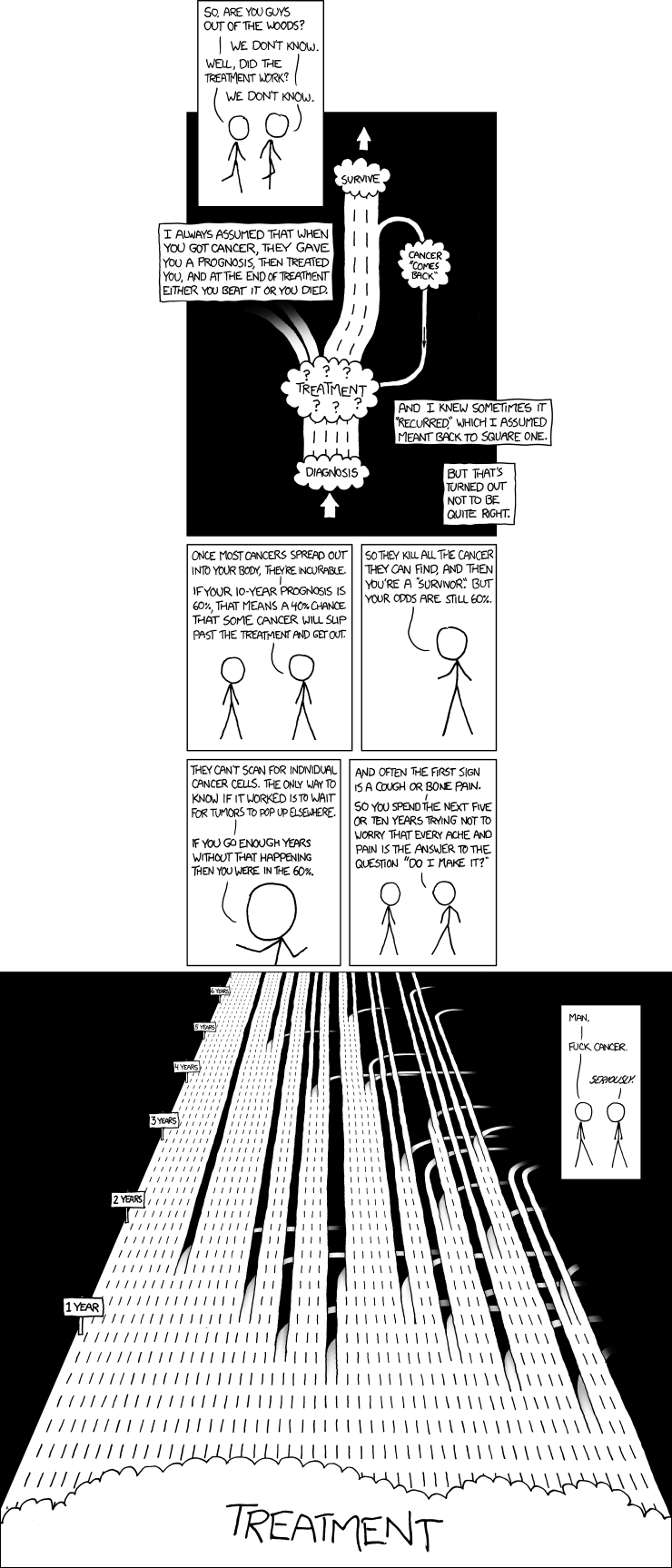
Randall Munroe’s comic ‘Lanes’ (xkcd nr. 931). From: xkcd.com/931